
By Elias Michael
REACH Ethiopia works on improving the performance of health extension workers (HEWs) on maternal health in Sidama Zone of the South Nation Nationalities and Peoples Region. This work is part of the REACHOUT consortium, an ambitious 5-year international research consortium funded by the European Commission. REACHOUT helps to understand and develop the role of close-to-community (CTC) providers working on improving the health status of communities in Africa and Asia. The aim of REACHOUT is to maximize the equity, effectiveness and efficiency of CTC services in rural areas and urban slums in six countries: Bangladesh, Ethiopia, Indonesia, Kenya, Malawi and Mozambique.
In 2013, a context analysis, consisting of a document review and a qualitative study in six districts of Sidama revealed that supervision of HEWs, referral and coordination and community engagement were the main areas for improvement of performance of HEWs. Therefore, a quality improvement (QI) intervention focusing on these areas was introduced in 2014. This marked the start of a QI cycle, in which the outcomes of the interventions were followed over the course of one year in one district, using observations, tracking registers and interviews with HEWs and women in the community.
The community engagement intervention
The community engagement part of the intervention was based on existing strategies and programmes in Ethiopia. As such, no new structures were introduced. Existing community engagement activities, related to pregnant women forums (PWFs) and health development army (HDA) leaders’ meetings were reviewed, adapted and included in an integrated refresher training of the HEWs. A PWF and a HDA leaders’ meeting guide were developed, in order to assist HEWs during these meetings. Sixty-five HEWs received the training and guides and were responsible for facilitating the intervention in the community. The intervention was supervised by health centre staff (the official supervisors of the HEWs) and REACH Ethiopia staff, and feedback about the implementation of the intervention was provided to HEWs.
What is the pregnant women forum?
Each health post, staffed by two HEWs, is supposed to hold one PWF per month. Pregnant women living in the community are expected to attend the PWF regularly. During the meeting, danger signs of pregnancy, advantages of antenatal care (ANC), institutional delivery, postnatal care (PNC) and cultural and other factors influencing mothers to access maternal health services are discussed and addressed as per the queries raised in the group. Every pregnant mother develops an individual birth plan with the ultimate goal of giving birth at the health facility. The PWF is led by a HEW, often in cooperation with a health professional, such as a midwife.
What is the health development army?
The HDA is an organized movement of the community, introduced nationwide in 2012.Through participatory learning and action meetings led by HEWs, communities are capacitated to take ownership of their own health. A Development Group is a community structure composed of 30 women representing their families. The women in each Development Group are clustered in one-to-five networks. The one-to-five networks develop their own health improvement plan which is further cascaded to each individual woman in the network. These plans contain individual targets in line with the Health Extension Programme. Members of the network implement and continuously monitor their performance with close follow-up and technical support from HEWs, during monthly HDAleaders’ meetings at the health post level.
Key findings
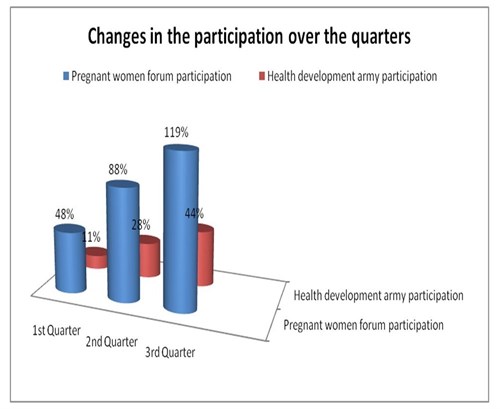
The participation for both types of meetings increased over time as a result of the intervention. The proportion of pregnant mothers who attended the PWF in the 1st, 2nd and 3rd quarters was 47.9%, 88% and 119% respectively. (The percentage above 100% shows that there is still a gap in information on the number of pregnant women in the community.) The proportion of HDA leaders who attended the HDA leaders’ meeting in the same period was 11%, 28% and 44%. In both community meetings, the level of participation shows a promising trend.
The HDA leaders also contributed to an increase in the identification of new pregnancies, thereby linking referral between the community and the HEWs. The percentage of pregnant women who came for care and were identified by the HDA increased from 43% to 85%. Generally, the ANC utilization figures went up, from 73% to77%. The institutional delivery increased from 79% to 83.3%. The community engagement activities could have contributed to this change, as illustrated by the following quotes:
"Health development army are always identifying pregnant women and report every week. When there were referral cases, they give a call to HEWs, and then we go to their home with ambulance. Whereas, when there is new pregnancy they inform to the leader of the team, then the leader would bring her to HEWs..." (Interview with HEW)
"The one-to-five leader encourages us a lot to deliver at the health facility. When our abdomen increases in size, she comes to us and asks us whether we are pregnant or not. If she gets a woman who is pregnant, she advices a lot so as to go to the health facility. She teaches us a lot." (Interview with woman in the community)
Of course, other parts of the REACH intervention, related to supervision and referral, could also have contributed towards the above mentioned improvements.
Besides the increase in identification of pregnancies and utilization of maternal health services, HEWs and community members felt there was increased knowledge and awareness about maternal health issues in the community. Some of the constraints as indicated by HEWs were absentees and the unfulfilled request for financial incentives by HDA leaders.
"These HDA leaders were previously voluntary community health workers. These guys previously got incentives one a three month or six months and have such habit. But now nothing at all; these people rumour such things saying health extension workers getting for themselves letting us to work for free. As this programme is a government concern some are working and some are not because of explained reasons" (Interview with HEW)
The issue of incentives was not posed as a problem for the PWF: women were willing to come and eager to discuss maternal health issues with each other. In some areas, HEWs and health centre staff provided the women tea and coffee, paid for with their own money. Support from the Kebele (the lowest administrative unit) administrator was mentioned as a facilitating factor for HDA leaders’ meetings, as it provided recognition for HDA leaders. However, this support was not available in all areas.
In 2016, REACH Ethiopia will implement a second QI cycle, with intensified community engagement elements, scaled up to five other districts.
Photo credit: Pregnant Women Forum held in Shebedino woreda, Nure Dulecha health post, by REACH Ethiopia
Recent news
- Practical training on e-health delivered by REACH Ethiopia, 23 March 2015
- Junior doctors in the UK are striking: How to motivate the health workforce, 25 February 2016
- Working with what we’ve got – an(other) reflection on human resources for health

This project is funded by the European Union.
